Recently, there has been shifting focus to topical and oral probiotics. So far, it has yielded promising and exciting results in the treatment of acne.
The propelling questions you may want to ask are, do probiotics help acne? How effective are they? Are they safe? Why is it necessary to consider probiotics in the treatment of acne?
Probiotics can be administered orally or topically (e.g as cream, lotion etc.). They are also used as adjuvant treatment to standard care.
Growing concerns with current medical treatment
You may have noticed that the focus has been gradually shifting to alternative and effective treatment for acne. This is largely due to growing concerns regarding the use of current conventional treatments for acne as follows;
- Antibiotics in the treatment of acne is increasingly associated with resistance, ineffectiveness, side effects and increasing risk for opportunistic infection due to disruption of skin microbiome.
- Isotretinoin has been known to cause serious side effects as well.
- Retinoic acids have been thought to cause disturbance in intestinal barrier leading to the gut permeability to Lipopolysaccharides (LPS) endotoxins. Note: LPS endotoxins can trigger inflammatory processes that can cause a variety of health issues.
Gut and skin microbiome – microbial balance
One of the ways probiotics exert its effect is by influencing the body’s microbiome – inclusive of the skin and gut.
What does microbiome mean? Microbiome is a collection of the genome of microbes present in your gut and skin. These microbes include bacteria, bacteriophage, fungi, protozoa and viruses.
A healthy microbiome helps you to reinforce your barrier immunity, while at same time protecting their ecological niche. They form a symbiotic relationship with humans – in simple words, a give and take relationship in a non-harmful way.
When a healthy microbiome or microbial balance is disturbed by a variety of processes such as invasion of other organisms that naturally do not exist in that niche or by temperature or other internal or external factors, then a disease process can occur.
So what are probiotics?
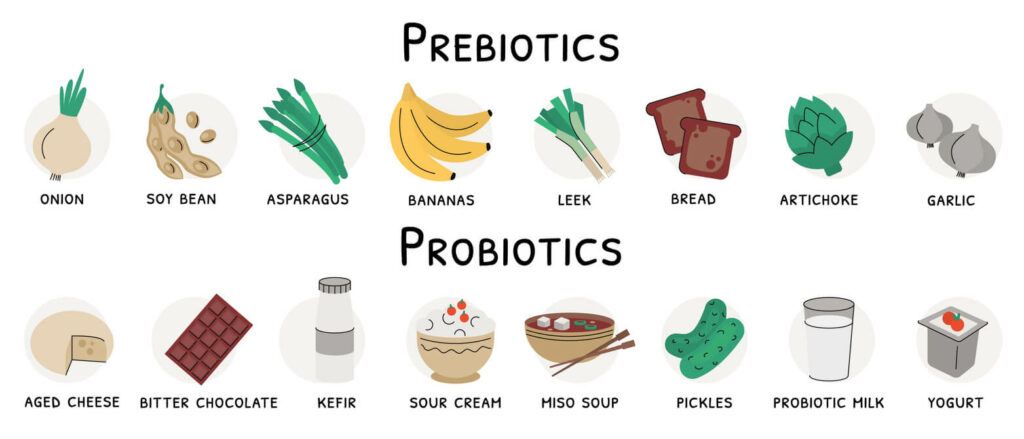
I’ll like to quickly mention that there are also prebiotics. These are certain food items that can help feed the beneficial microbes in your gut while promoting their growth and activity.
But our focus is on probiotics!
Probiotics are considered to be live non-harmful micro-organisms that will help you health-wise in a number of ways when administered orally or topically, as considered in this article.
Selection criteria for probiotics for skin and gut are;
Skin Application criteria
- They include adhesion to keratin, ability to prevent adhesion of harmful bacteria and exhibition of antimicrobial property.
Gut probiotic criteria
- adhesion to intestinal mucous, as well as acid and bile resistance of the gut.
5 examples of non-harmful microbes with probiotic benefits;
You may recognize the following microbes with probiotic benefits, though there are more;
- Dairy Propionic Acid Bacteria (PAB)
- Saccharomyces boulardii
- Yeast or lactic acid bacteria
- Lactobacillus species
- Bifidobacterium species.
Some general benefits of probiotics
- Used treat skin conditions such as acne,
- Used to treat acute diarrhea.
- Improves bowel function and decreases constipation.
- Helps to minimize systemic oxidative stress due to intense physical activity (e.g Lactobacillus rhamnosus and Lactobacillus paracasei).
- Helps to improve mental health by decreasing proliferation of bacteria in the small intestine. Bacteria overgrowth in small intestine has been thought to be 10 times more common in acne sufferers than in people without acne. This is thought to result in acne related psychological stress.
- Helps to improve immune system
- Can help protect and shield the skin.
- Reduces inflammation and lesion count in acne
- Improves skin complexion.
Relevance of probiotics in acne

Anti-microbial
Propionibacteria acne (P. acne), more recently known as Cutibacterium acne (C. acne). Naturally found in the skin, adheres to keratin and exhibits a broad range of antimicrobial activity (e.g. anti fungal activity against Candida albicans).
Proliferation of P. acne is thought to contribute or exacerbate acne
Certain probiotics have displayed antimicrobial effects against P. acne. For example, Lactobacillus reuteri produce organic acid which is thought to exert its topical antimicrobial effects against P. acne.
Androgen modulator
Increased production of androgenic hormones play a crucial role in the pathogenesis of acne, the gut microbiome can influence the metabolism of androgen in the intestine.
Probiotics exert their effect by helping to restore the guts microbiome – thus modulating intestinal androgen metabolism.
Sebum production
Altered composition or increased sebum product play a key role in the pathogenesis of acne. P. acne can trigger inflammation and increased sebum production.
Probiotics have been shown to inhibit P. acne that can trigger increase in sebum. This is a relevant consideration in the treatment of acne
Ceramide
Ceramide is thought to be low in people with acne. During winter, there could be loss of ceramide as well. Some Sphingolipid ceramides (e.g. phytosphingosine) exert antimicrobial effect on the skin and against P. acne. Ceremide also helps to prevent dryness by trapping moisture.
When probiotic (such as Streptococcus thermophilus found in yogurt) is applied to the skin as cream for 7 days, it can help to increase ceremide production which can in turn help reduce papules and pustules, restore healthy fat and counter the effects caused by acne therapies.
Glycemic control
Foods with high glycemic index or glycemic load (GI or GL), high fat and low fiber diets can contribute to or exacerbate acne.
When you make such poor dietary choices, you loose bifidobacteria in your gut. This makes your gut more permeable, allowing LPS endotoxins to get into your systemic circulation. The result of this is in insulin resistance, increased glucose level and subsequent increase in insulin-like growth factor-1 (IGF-1)
Probiotics such as Bifidobacterium lactis (when taken orally) can help to improve insulin sensitivity and increase uptake of glucose even when high fat diets are consumed. B. lactis does this by hindering access of LPS toxins to your systemic circulation.
Anti-Inflammation
inflammatory mediators such as cytokines that occur during inflammatory processes can trigger acne.
When probiotic lotion of Enterococcus faecalis was applied to the skin can regulate inflammatory cytokines in the skin. This was shown to reduce inflammation and lesion count by 50% in 8 weeks.
Also, probiotic such as Streptococcus salvarius can inhibit inflammation in the epithelial cells and keratinocytes of the skin when applied topically
“Acne personality”
Stress cotisol can make acne worse and enhance bacteria overgrowth in your small intestine. Bacteria overgrowth can in turn hinder your small intestine from absorbing micro nutrients, vitamin B, carbohydrates and protein.
Daily probiotics supplements help with reducing stress cotisol as well as anxiety, depression and anger. Psychological stress contributes to breakouts or exacerbation of acne. An example of such probiotics is an oral administration of combined non-harmful bacteria – L. helveticus and B. longum.
Other psychological impairments such as anxiety, depression and anger have also been noted to be high among acne sufferers. Probiotics can help to improve such acne related psychological impairments.
Fermented milk (in yoghort) and beverage benefits

Fermented milk
IGF-1 is 4 times less in fermented milk (in yoghurt) compared to skimmed milk because during the fermentation process probiotic bacteria (e.g lactobacilli) is added. This utilizes IGF-1 which is considered to make acne worse.
The use of yoghurt a key ingredient in modern skin care has proven to be highly effective and tolerable
Fermented milk does two things: 1) increases the amount of systemic antioxidant enzyme and their activity 2) improves fasting blood glucose
Fermented beverage
Lactobacillus fermented dairy beverage can significantly improve acne over 12 weeks when orally taken regularly.
I like to hear your thoughts. Leave your comment below and I’ll get back ASAP
References
Belkaid, Y. and Hand, T. Role of the Microbiota in Immunity and inflammation. Cell Author Manuscripts. 2015. 157(1): 121-141. doi:10.1016/j.cell.2014.03.011
Bowe, W., Patel, N. B. and Logan, A. C. Acne vulgaris, probiotics and the gut-brain-skin axis: from anecdote to translational medicine. Beneficial Microbes. 2014. 5(2): 185-199(15). https://doi.org/10.3920/BM2012.0060
Collden, H., et al. The gut microbiota is a major regulator of androgen metabolism in intestinal contents. Endocrine and Metabolism. 2019. 317(6); E1182-E1192. https://doi.org/10.1152/ajpendo.00338.2019
Eloe-Fadrosh, E. A. and Rasko, D. A. The Human Microbiome: From Symbiosis to Pathogenesis. HHS Author Manuscripts. 2014. 64: 145-163. doi:10.1146/annurev-med-010312-133513
Kober, M. and Bowe, W. P. The effect of probiotics on immune regulation, acne, and photoaging. Int J Womens Dermatol. 2015. 1(2): 85-89. doi:10.1016/j.ijwd.2015.02.001
Lee, Y. B., Byun, E. J. and Kim, H. S. Potential Role of the Microbiome in Acne: A Comprehensive Review. J Clin Med. 2019. 8(7): 987. doi:10.3390/jcm8070987
Ouwehand, A. C., Batsman, A. and Salminen, S. Probiotics for the skin: a new area of potential application? Letters In Applied Microbiology. 2003. 36(5): 327-331. https://doi.org/10.1046/j.1472-765X.2003.01319.x
Williams, N. T. Probiotics. American Journal of Health-System Pharmacy. 2010. 67(6): 449-458. https://doi.org/10.2146/ajhp090168
Yang, J. The Human Microbiome Project: Extending the definition of what constitutes a human. National Human Genome Research Institute. 2012. The Human Microbiome Project: Extending the definition of what constitutes a human (genome.gov)